.What does RCH stand for?
1. Reproductive and Complete Health
2. Regional and Central Healthcare
3. Reproductive and Child Healthcare
4. Reproductive and Cumulative Health
.
.
Answer ▽ ✅Verified
3. Reproductive and Child Healthcare
REPRODUCTIVE HEALTH – PROBLEMS AND
STRATEGIES
India was amongst the first countries in the world toinitiate action plans and programmes at a national level
to attain total reproductive health as a social goal.
These programmes called ‘family planning’ were
initiated in 1951 and were periodically assessed over
the past decades. Improved programmes covering wider
reproduction-related areas are currently in operation under the
popular name ‘Reproductive and Child Health Care (RCH) programmes’.
Creating awareness among people about various reproduction related
aspects and providing facilities and support for building up a
reproductively healthy society are the major tasks under these
programmes.
With the help of audio-visual and the print-media governmental and
non-governmental agencies have taken various steps to create awareness
among the people about reproduction-related aspects. Parents, other
close relatives, teachers and friends, also have a major role in the
dissemination of the above information. Introduction of sex education
in schools should also be encouraged to provide right information to
the young so as to discourage children from believing in myths and
having misconceptions about sex-related aspects. Proper information
about reproductive organs, adolescence and related changes, safe and
hygienic sexual practices, sexually transmitted diseases (STD), AIDS,
etc., would help people, especially those in the adolescent age group to
lead a reproductively healthy life. Educating people, especially fertile
couples and those in marriageable age group, about available birth
control options, care of pregnant mothers, post-natal care of the mother
and child, importance of breast feeding, equal opportunities for the male
and the female child, etc., would address the importance of bringing up
socially conscious healthy families of desired size. Awareness of problems
due to uncontrolled population growth, social evils like sex-abuse and
sex-related crimes, etc., need to be created to enable people to think
and take up necessary steps to prevent them and thereby build up a
socially responsible and healthy society.
⬆️Prev____@organised notes_____Next⬇️
.The ideal contraceptive for females who want to delay pregnancy and/or space children is:
1 Barrier contraceptive
2. Periodic abstinence
3. IUD
4. Hormonal pills
.
.
Answer ▽ ✅Verified
3. IUD
BIRTH CONTROL
families by using various contraceptive methods.
An ideal contraceptive should be user-friendly, easily available,
effective and reversible with no or least side-effects. It also should in no
way interfere with the sexual drive, desire and/or the sexual act of the
user. A wide range of contraceptive methods are presently available which
could be broadly grouped into the following categories, namely
Natural/Traditional, Barrier, IUDs, Oral contraceptives, Injectables,
Implants and Surgical methods.
Natural methods work on the principle of avoiding chances of ovum
and sperms meeting. Periodic abstinence is one such method in which
the couples avoid or abstain from coitus from day 10 to 17 of the menstrual
cycle when ovulation could be expected. As chances of fertilisation are
very high during this period, it is called the fertile period. Therefore, by
abstaining from coitus during this period, conception could
be prevented. Withdrawal or coitus interruptus is another
method in which the male partner withdraws his penis from
the vagina just before ejaculation so as to avoid
insemination. Lactational amenorrhea (absence of
menstruation) method is based on the fact that ovulation
and therefore the cycle do not occur during the period of
intense lactation following parturition. Therefore, as long
as the mother breast-feeds the child fully, chances of
conception are almost nil. However, this method has been
reported to be effective only upto a maximum period of six
months following parturition. As no medicines or devices
are used in these methods, side effects are almost nil.
Chances of failure, though, of this method are also high.
In barrier methods, ovum and sperms are prevented
from physically meeting with the help of barriers. Such
methods are available for both males and females.
Condoms (Figure 4.1 a, b) are barriers made of thin rubber/
latex sheath that are used to cover the penis in the male or
vagina and cervix in the female, just before coitus so that
the ejaculated semen would not enter into the female
reproductive tract. This can prevent conception. ‘Nirodh’ is
a popular brand of condom for the male. Use of condoms
has increased in recent years due to its additional benefit of
protecting the user from contracting STIs and AIDS. Both
the male and the female condoms are disposable, can be
self-inserted and thereby gives privacy to the user.
Diaphragms, cervical caps and vaults are also barriers
made of rubber that are inserted into the female reproductive
tract to cover the cervix during coitus. They prevent
conception by blocking the entry of sperms through the
cervix. They are reusable. Spermicidal creams, jellies and
foams are usually used alongwith these barriers to increase
their contraceptive efficiency.
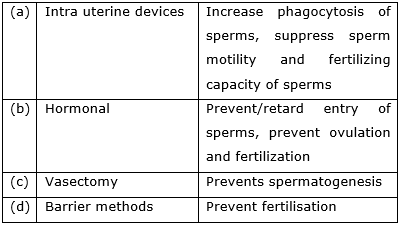
Another effective and popular method is the use of Intra Uterine
Devices (IUDs). These devices are inserted by doctors or expert nurses
in the uterus through vagina. These Intra Uterine Devices are presently
available as the non-medicated IUDs (e.g., Lippes loop), copper releasing
IUDs (CuT, Cu7, Multiload 375) and the hormone releasing IUDs
(Progestasert, LNG-20) (Figure 4.2). IUDs increase phagocytosis of sperms
within the uterus and the Cu ions released suppress sperm motility and
the fertilising capacity of sperms. The hormone releasing IUDs, in addition
make the uterus unsuitable for implantation and the
cervix hostile to the sperms. IUDs are ideal contraceptives
for the females who want to delay pregnancy and/or space
children. It is one of most widely accepted methods of
contraception in India.
Oral administration of small doses of either progestogens
or progestogen–estrogen combinations is another
contraceptive method used by the females. They are used
in the form of tablets and hence are popularly called the
pills. Pills have to be taken daily for a period of 21 days
starting preferably within the first five days of menstrual
cycle. After a gap of 7 days (during which menstruation
occurs) it has to be repeated in the same pattern till the female desires to
prevent conception. They inhibit ovulation and implantation as well as
alter the quality of cervical mucus to prevent/retard entry of sperms. Pills
are very effective with lesser side effects and are well accepted by the females.
Saheli –the new oral contraceptive for the females contains a non-steroidal
preparation. It is a ‘once a week’ pill with very few side effects and high
contraceptive value.
Progestogens alone or in combination with estrogen can also be used
by females as injections or implants under the skin (Figure 4.3). Their
mode of action is similar to that of pills and their effective periods are
much longer. Administration of progestogens or progestogen-estrogen
combinations or IUDs within 72 hours of coitus have been found to be
very effective as emergency contraceptives as they could be used to avoid
possible pregnancy due to rape or casual unprotected intercourse.
Surgical methods, also called sterilisation, are generally advised for
the male/female partner as a terminal method
⬆️Prev____@organised notes_____Next⬇️
.ART [used to help infertile couples] stands for:
1. Assisted Reproductive Technologies
2. Artificial Reproductive Technologies
3. Augmented Reproductive Technologies
4. Anomalous Reproductive Technologies
.
.
Answer ▽ ✅Verified
1. Assisted Reproductive Technologies
INFERTILITY
infertility. A large number of couples all over the world including India
are infertile, i.e., they are unable to produce children inspite of unprotected
sexual co-habitation. The reasons for this could be many–physical,
congenital, diseases, drugs, immunological or even psychological.
In India, often the female is blamed for the couple being childless, but
more often than not, the problem lies in the male partner. Specialised
health care units (infertility clinics, etc.) could help in diagnosis and
corrective treatment of some of these disorders and enable these couples to
have children. However, where such corrections are not possible, the couples
could be assisted to have children through certain special techniques
commonly known as assisted reproductive technologies (ART).
In vitro fertilisation (IVF–fertilisation outside the body in almost
similar conditions as that in the body) followed by embryo transfer (ET)
is one of such methods. In this method, popularly known as test tube
baby programme, ova from the wife/donor (female) and sperms from the
husband/donor (male) are collected and are induced to form zygote under
simulated conditions in the laboratory. The zygote or early embryos (with
upto 8 blastomeres) could then be transferred into the fallopian tube
(ZIFT–zygote intra fallopian transfer) and embryos with more than
8 blastomeres, into the uterus (IUT – intra uterine transfer), to complete
its further development. Embryos formed by in-vivo fertilisation (fusion
of gametes within the female) also could be used for such transfer to assist
those females who cannot conceive.
Transfer of an ovum collected from a donor into the fallopian tube
(GIFT – gamete intra fallopian transfer) of another female who cannot
produce one, but can provide suitable environment for fertilisation and
further development is another method attempted. Intra cytoplasmic
sperm injection (ICSI) is another specialised procedure to form an embryo
in the laboratory in which a sperm is directly injected into the ovum.
Infertility cases either due to inability of the male partner to inseminate
the female or due to very low sperm counts in the ejaculates, could be
corrected by artificial insemination (AI) technique. In this technique,
the semen collected either from the husband or a healthy donor is artificially
introduced either into the vagina or into the uterus (IUI – intra-uterine
insemination) of the female.
Though options are many, all these techniques require extremely high
precision handling by specialised professionals and expensive
instrumentation. Therefore, these facilities are presently available only in
very few centres in the country. Obviously their benefits is affordable to
only a limited number of people. Emotional, religious and social factors
are also deterrents in the adoption of these methods. Since the ultimate
aim of all these procedures is to have children, in India we have so many
orphaned and destitute children, who would probably not survive till
maturity, unless taken care of. Our laws permit legal adoption and it is
as yet, one of the best methods for couples looking for parenthood.
⬆️Prev____@organised notes_____Next⬇️
.Vasectomies:
1. Inhibit testosterone production
2. Prevent sperm from entering the semen
3. Inhibit spem production
4. Interfere with male potency
.
.
Answer ▽ ✅Verified
2. Prevent sperm from entering the semen
Surgical intervention blocks gamete transport and thereby
prevent conception. Sterilisation procedure in the male is called ‘vasectomy’
In vasectomy, a small part of the vas
deferens is removed or tied up through a small incision on the scrotum
⬆️Prev____@organised notes_____Next⬇️
.The function of copper ions in copper releasing IUD’s is
(1) they suppress sperm motility and fertilising capacity of sperms
(2) they inhibit gametogenesis
(3) they make uterus unsuitable for implantation
(4) they inhibit ovulation
.
.
Answer ▽ ✅Verified
(1) they suppress sperm motility and fertilising capacity of sperms
⬆️Prev____@organised notes_____Next⬇️
.Which of the following is hormone-releasing IUD?
(1) LNG-20
(2) Multiload-375
(3) Lippes loop
(4) Cu-7
.
.
Answer ▽ ✅Verified
(1) LNG-20
⬆️Prev____@organised notes_____Next⬇️
.A childless couple can be assisted to have a child through a technique called GIFT. The
full form of this technique is
1. Gamete Inseminated Fallooian Transfer
2. Gamete Intra Fallopian Transfer
3. Gamete Internal Fertilization and Transfer
4. Germ Cell Internal Fallopian Transfer
.
.
Answer ▽ ✅Verified
2. Gamete Intra Fallopian Transfer
INFERTILITY
infertility. A large number of couples all over the world including India
are infertile, i.e., they are unable to produce children inspite of unprotected
sexual co-habitation. The reasons for this could be many–physical,
congenital, diseases, drugs, immunological or even psychological.
In India, often the female is blamed for the couple being childless, but
more often than not, the problem lies in the male partner. Specialised
health care units (infertility clinics, etc.) could help in diagnosis and
corrective treatment of some of these disorders and enable these couples to
have children. However, where such corrections are not possible, the couples
could be assisted to have children through certain special techniques
commonly known as assisted reproductive technologies (ART).
In vitro fertilisation (IVF–fertilisation outside the body in almost
similar conditions as that in the body) followed by embryo transfer (ET)
is one of such methods. In this method, popularly known as test tube
baby programme, ova from the wife/donor (female) and sperms from the
husband/donor (male) are collected and are induced to form zygote under
simulated conditions in the laboratory. The zygote or early embryos (with
upto 8 blastomeres) could then be transferred into the fallopian tube
(ZIFT–zygote intra fallopian transfer) and embryos with more than
8 blastomeres, into the uterus (IUT – intra uterine transfer), to complete
its further development. Embryos formed by in-vivo fertilisation (fusion
of gametes within the female) also could be used for such transfer to assist
those females who cannot conceive.
Transfer of an ovum collected from a donor into the fallopian tube
(GIFT – gamete intra fallopian transfer) of another female who cannot
produce one, but can provide suitable environment for fertilisation and
further development is another method attempted. Intra cytoplasmic
sperm injection (ICSI) is another specialised procedure to form an embryo
in the laboratory in which a sperm is directly injected into the ovum.
Infertility cases either due to inability of the male partner to inseminate
the female or due to very low sperm counts in the ejaculates, could be
corrected by artificial insemination (AI) technique. In this technique,
the semen collected either from the husband or a healthy donor is artificially
introduced either into the vagina or into the uterus (IUI – intra-uterine
insemination) of the female.
Though options are many, all these techniques require extremely high
precision handling by specialised professionals and expensive
instrumentation. Therefore, these facilities are presently available only in
very few centres in the country. Obviously their benefits is affordable to
only a limited number of people. Emotional, religious and social factors
are also deterrents in the adoption of these methods. Since the ultimate
aim of all these procedures is to have children, in India we have so many
orphaned and destitute children, who would probably not survive till
maturity, unless taken care of. Our laws permit legal adoption and it is
as yet, one of the best methods for couples looking for parenthood.
⬆️Prev____@organised notes_____Next⬇️
.Which of the following is not a sexually transmitted disease?
1. Syphilis
2. Acquired ImmunoDeficiency Syndrome (AIDS)
3. Trichomoniasis
4. Encephalitis
.
.
Answer ▽ ✅Verified
4. Encephalitis
Infections or diseases which are transmitted through sexual intercourse
are collectively called sexually transmitted infections (STI) or venereal
diseases (VD) or reproductive tract infections (RTI). Gonorrhoea, syphilis,
genital herpes, chlamydiasis, genital warts, trichomoniasis, hepatitis-B
and of course, the most discussed infection in the recent years, HIV leading
to AIDS are some of the common STIs. Among these, HIV infection is
most dangerous .
Some of these infections like hepatitis–B and HIV can also be
transmitted by sharing of injection needles, surgical instruments, etc.,
with infected persons, transfusion of blood, or from an infected mother to
the foetus too. Except for hepatitis-B, genital herpes and HIV infections,
other diseases are completely curable if detected early and treated
properly. Early symptoms of most of these are minor and include itching,
fluid discharge, slight pain, swellings, etc., in the genital region. Infected
females may often be asymptomatic and hence, may remain undetected
for long. Absence or less significant symptoms in the early stages of
infection and the social stigma attached to the STIs, deter the infected
persons from going for timely detection and proper treatment. This could
lead to complications later, which include pelvic inflammatory diseases
(PID), abortions, still births, ectopic pregnancies, infertility or even cancer
of the reproductive tract. STIs are a major threat to a healthy society.
Therefore, prevention or early detection and cure of these diseases are
given prime consideration under the reproductive health-care
programmes. Though all persons are vulnerable to these infections, their
incidences are reported to be very high among persons in the age group
of 15-24 years – the age group to which you also belong. There is no
reason to panic because prevention is possible. One could be free of these
infections by following the simple principles given below:
(i) Avoid sex with unknown partners/multiple partners.
(ii) Always try to use condoms during coitus.
(iii) In case of doubt, one should go to a qualified doctor for early
detection and get complete treatment if diagnosed with infection.
⬆️Prev____@organised notes_____Next⬇️
.Assisted reproductive technology, IVF involves transfer of
1. ovum into the Fallopian tube
2. embryo upto 8-celled stage into the Fallopian tube
3. embryo upto 8-celled stage into the uterus
4. embryo with 16 balastomeres into the Fallopian tube
.
.
Answer ▽ ✅Verified
2. embryo upto 8-celled stage into the Fallopian tube
INFERTILITY
infertility. A large number of couples all over the world including India
are infertile, i.e., they are unable to produce children inspite of unprotected
sexual co-habitation. The reasons for this could be many–physical,
congenital, diseases, drugs, immunological or even psychological.
In India, often the female is blamed for the couple being childless, but
more often than not, the problem lies in the male partner. Specialised
health care units (infertility clinics, etc.) could help in diagnosis and
corrective treatment of some of these disorders and enable these couples to
have children. However, where such corrections are not possible, the couples
could be assisted to have children through certain special techniques
commonly known as assisted reproductive technologies (ART).
In vitro fertilisation (IVF–fertilisation outside the body in almost
similar conditions as that in the body) followed by embryo transfer (ET)
is one of such methods. In this method, popularly known as test tube
baby programme, ova from the wife/donor (female) and sperms from the
husband/donor (male) are collected and are induced to form zygote under
simulated conditions in the laboratory. The zygote or early embryos (with
upto 8 blastomeres) could then be transferred into the fallopian tube
(ZIFT–zygote intra fallopian transfer) and embryos with more than
8 blastomeres, into the uterus (IUT – intra uterine transfer), to complete
its further development. Embryos formed by in-vivo fertilisation (fusion
of gametes within the female) also could be used for such transfer to assist
those females who cannot conceive.
Transfer of an ovum collected from a donor into the fallopian tube
(GIFT – gamete intra fallopian transfer) of another female who cannot
produce one, but can provide suitable environment for fertilisation and
further development is another method attempted. Intra cytoplasmic
sperm injection (ICSI) is another specialised procedure to form an embryo
in the laboratory in which a sperm is directly injected into the ovum.
Infertility cases either due to inability of the male partner to inseminate
the female or due to very low sperm counts in the ejaculates, could be
corrected by artificial insemination (AI) technique. In this technique,
the semen collected either from the husband or a healthy donor is artificially
introduced either into the vagina or into the uterus (IUI – intra-uterine
insemination) of the female.
Though options are many, all these techniques require extremely high
precision handling by specialised professionals and expensive
instrumentation. Therefore, these facilities are presently available only in
very few centres in the country. Obviously their benefits is affordable to
only a limited number of people. Emotional, religious and social factors
are also deterrents in the adoption of these methods. Since the ultimate
aim of all these procedures is to have children, in India we have so many
orphaned and destitute children, who would probably not survive till
maturity, unless taken care of. Our laws permit legal adoption and it is
as yet, one of the best methods for couples looking for parenthood.
⬆️Prev____@organised notes_____Next⬇️
.The test-tube baby programme employs which one of the following techniques?
1. Intra Cytoplasmic Sperm Injection (ICSI)
2. Intra Uterine Insemination (IUI)
3. Gamete Intra Fallopian Transfer (GIFT)
4. Zygote Intra Fallopian Transfer (ZIFT)
.
.
Answer ▽ ✅Verified
4. Zygote Intra Fallopian Transfer (ZIFT)
INFERTILITY
infertility. A large number of couples all over the world including India
are infertile, i.e., they are unable to produce children inspite of unprotected
sexual co-habitation. The reasons for this could be many–physical,
congenital, diseases, drugs, immunological or even psychological.
In India, often the female is blamed for the couple being childless, but
more often than not, the problem lies in the male partner. Specialised
health care units (infertility clinics, etc.) could help in diagnosis and
corrective treatment of some of these disorders and enable these couples to
have children. However, where such corrections are not possible, the couples
could be assisted to have children through certain special techniques
commonly known as assisted reproductive technologies (ART).
In vitro fertilisation (IVF–fertilisation outside the body in almost
similar conditions as that in the body) followed by embryo transfer (ET)
is one of such methods. In this method, popularly known as test tube
baby programme, ova from the wife/donor (female) and sperms from the
husband/donor (male) are collected and are induced to form zygote under
simulated conditions in the laboratory. The zygote or early embryos (with
upto 8 blastomeres) could then be transferred into the fallopian tube
(ZIFT–zygote intra fallopian transfer) and embryos with more than
8 blastomeres, into the uterus (IUT – intra uterine transfer), to complete
its further development. Embryos formed by in-vivo fertilisation (fusion
of gametes within the female) also could be used for such transfer to assist
those females who cannot conceive.
Transfer of an ovum collected from a donor into the fallopian tube
(GIFT – gamete intra fallopian transfer) of another female who cannot
produce one, but can provide suitable environment for fertilisation and
further development is another method attempted. Intra cytoplasmic
sperm injection (ICSI) is another specialised procedure to form an embryo
in the laboratory in which a sperm is directly injected into the ovum.
Infertility cases either due to inability of the male partner to inseminate
the female or due to very low sperm counts in the ejaculates, could be
corrected by artificial insemination (AI) technique. In this technique,
the semen collected either from the husband or a healthy donor is artificially
introduced either into the vagina or into the uterus (IUI – intra-uterine
insemination) of the female.
Though options are many, all these techniques require extremely high
precision handling by specialised professionals and expensive
instrumentation. Therefore, these facilities are presently available only in
very few centres in the country. Obviously their benefits is affordable to
only a limited number of people. Emotional, religious and social factors
are also deterrents in the adoption of these methods. Since the ultimate
aim of all these procedures is to have children, in India we have so many
orphaned and destitute children, who would probably not survive till
maturity, unless taken care of. Our laws permit legal adoption and it is
as yet, one of the best methods for couples looking for parenthood.
⬆️Prev____@organised notes_____Next⬇️
.Contraceptive oral pills help in birth control by
(1) killing the sperms in uterus
(2) preventing implantation
(3) preventing ovulation
(4) both (b) and (c).
.
.
Answer ▽ ✅Verified
(4) both (b) and (c).
BIRTH CONTROL
families by using various contraceptive methods.
An ideal contraceptive should be user-friendly, easily available,
effective and reversible with no or least side-effects. It also should in no
way interfere with the sexual drive, desire and/or the sexual act of the
user. A wide range of contraceptive methods are presently available which
could be broadly grouped into the following categories, namely
Natural/Traditional, Barrier, IUDs, Oral contraceptives, Injectables,
Implants and Surgical methods.
Natural methods work on the principle of avoiding chances of ovum
and sperms meeting. Periodic abstinence is one such method in which
the couples avoid or abstain from coitus from day 10 to 17 of the menstrual
cycle when ovulation could be expected. As chances of fertilisation are
very high during this period, it is called the fertile period. Therefore, by
abstaining from coitus during this period, conception could
be prevented. Withdrawal or coitus interruptus is another
method in which the male partner withdraws his penis from
the vagina just before ejaculation so as to avoid
insemination. Lactational amenorrhea (absence of
menstruation) method is based on the fact that ovulation
and therefore the cycle do not occur during the period of
intense lactation following parturition. Therefore, as long
as the mother breast-feeds the child fully, chances of
conception are almost nil. However, this method has been
reported to be effective only upto a maximum period of six
months following parturition. As no medicines or devices
are used in these methods, side effects are almost nil.
Chances of failure, though, of this method are also high.
In barrier methods, ovum and sperms are prevented
from physically meeting with the help of barriers. Such
methods are available for both males and females.
Condoms (Figure 4.1 a, b) are barriers made of thin rubber/
latex sheath that are used to cover the penis in the male or
vagina and cervix in the female, just before coitus so that
the ejaculated semen would not enter into the female
reproductive tract. This can prevent conception. ‘Nirodh’ is
a popular brand of condom for the male. Use of condoms
has increased in recent years due to its additional benefit of
protecting the user from contracting STIs and AIDS. Both
the male and the female condoms are disposable, can be
self-inserted and thereby gives privacy to the user.
Diaphragms, cervical caps and vaults are also barriers
made of rubber that are inserted into the female reproductive
tract to cover the cervix during coitus. They prevent
conception by blocking the entry of sperms through the
cervix. They are reusable. Spermicidal creams, jellies and
foams are usually used alongwith these barriers to increase
their contraceptive efficiency.
Another effective and popular method is the use of Intra Uterine
Devices (IUDs). These devices are inserted by doctors or expert nurses
in the uterus through vagina. These Intra Uterine Devices are presently
available as the non-medicated IUDs (e.g., Lippes loop), copper releasing
IUDs (CuT, Cu7, Multiload 375) and the hormone releasing IUDs
(Progestasert, LNG-20) (Figure 4.2). IUDs increase phagocytosis of sperms
within the uterus and the Cu ions released suppress sperm motility and
the fertilising capacity of sperms. The hormone releasing IUDs, in addition
make the uterus unsuitable for implantation and the
cervix hostile to the sperms. IUDs are ideal contraceptives
for the females who want to delay pregnancy and/or space
children. It is one of most widely accepted methods of
contraception in India.
Oral administration of small doses of either progestogens
or progestogen–estrogen combinations is another
contraceptive method used by the females. They are used
in the form of tablets and hence are popularly called the
pills. Pills have to be taken daily for a period of 21 days
starting preferably within the first five days of menstrual
cycle. After a gap of 7 days (during which menstruation
occurs) it has to be repeated in the same pattern till the female desires to
prevent conception. They inhibit ovulation and implantation as well as
alter the quality of cervical mucus to prevent/retard entry of sperms. Pills
are very effective with lesser side effects and are well accepted by the females.
Saheli –the new oral contraceptive for the females contains a non-steroidal
preparation. It is a ‘once a week’ pill with very few side effects and high
contraceptive value.
Progestogens alone or in combination with estrogen can also be used
by females as injections or implants under the skin (Figure 4.3). Their
mode of action is similar to that of pills and their effective periods are
much longer. Administration of progestogens or progestogen-estrogen
combinations or IUDs within 72 hours of coitus have been found to be
very effective as emergency contraceptives as they could be used to avoid
possible pregnancy due to rape or casual unprotected intercourse.
Surgical methods, also called sterilisation, are generally advised for
the male/female partner as a terminal method
⬆️Prev____@organised notes_____Next⬇️
.When were family planning programmes initiated in India?
(1) 1948
(2) 1962
(3) 1959
(4) 1951
.
.
Answer ▽ ✅Verified
(4) 1951
India was amongst the first countries in the world to
initiate action plans and programmes at a national level
to attain total reproductive health as a social goal.
These programmes called ‘family planning’ were
initiated in 1951 and were periodically assessed over
the past decades. Improved programmes covering wider
reproduction-related areas are currently in operation under the
popular name ‘Reproductive and Child Health Care (RCH) programmes’.
Creating awareness among people about various reproduction related
aspects and providing facilities and support for building up a
reproductively healthy society are the major tasks under these
programmes.
With the help of audio-visual and the print-media governmental and
non-governmental agencies have taken various steps to create awareness
among the people about reproduction-related aspects. Parents, other
close relatives, teachers and friends, also have a major role in the
dissemination of the above information. Introduction of sex education
in schools should also be encouraged to provide right information to
the young so as to discourage children from believing in myths and
having misconceptions about sex-related aspects. Proper information
about reproductive organs, adolescence and related changes, safe and
hygienic sexual practices, sexually transmitted diseases (STD), AIDS,
etc., would help people, especially those in the adolescent age group to
lead a reproductively healthy life. Educating people, especially fertile
couples and those in marriageable age group, about available birth
control options, care of pregnant mothers, post-natal care of the mother
and child, importance of breast feeding, equal opportunities for the male
and the female child, etc., would address the importance of bringing up
socially conscious healthy families of desired size. Awareness of problems
due to uncontrolled population growth, social evils like sex-abuse and
sex-related crimes, etc., need to be created to enable people to think
and take up necessary steps to prevent them and thereby build up a
socially responsible and healthy society.
⬆️Prev____@organised notes_____Next⬇️
.What is the full form of RCH?
(1) Reproductive and Child Health Care
(2) Reproduction, Contraception and Health
(3) Reproduction and Child Health
(4) None of these
.
.
Answer ▽ ✅Verified
(1) Reproductive and Child Health Care
India was amongst the first countries in the world to
initiate action plans and programmes at a national level
to attain total reproductive health as a social goal.
These programmes called ‘family planning’ were
initiated in 1951 and were periodically assessed over
the past decades. Improved programmes covering wider
reproduction-related areas are currently in operation under the
popular name ‘Reproductive and Child Health Care (RCH) programmes’.
Creating awareness among people about various reproduction related
aspects and providing facilities and support for building up a
reproductively healthy society are the major tasks under these
programmes.
With the help of audio-visual and the print-media governmental and
non-governmental agencies have taken various steps to create awareness
among the people about reproduction-related aspects. Parents, other
close relatives, teachers and friends, also have a major role in the
dissemination of the above information. Introduction of sex education
in schools should also be encouraged to provide right information to
the young so as to discourage children from believing in myths and
having misconceptions about sex-related aspects. Proper information
about reproductive organs, adolescence and related changes, safe and
hygienic sexual practices, sexually transmitted diseases (STD), AIDS,
etc., would help people, especially those in the adolescent age group to
lead a reproductively healthy life. Educating people, especially fertile
couples and those in marriageable age group, about available birth
control options, care of pregnant mothers, post-natal care of the mother
and child, importance of breast feeding, equal opportunities for the male
and the female child, etc., would address the importance of bringing up
socially conscious healthy families of desired size. Awareness of problems
due to uncontrolled population growth, social evils like sex-abuse and
sex-related crimes, etc., need to be created to enable people to think
and take up necessary steps to prevent them and thereby build up a
socially responsible and healthy society.
⬆️Prev____@organised notes_____Next⬇️
.Where was "Saheli" developed?
(1) Indian Council of Medical Research, New Delhi
(2) Central Drug Research Institute, Lucknow
(3) All India Institute of Medical Sciences, New Delhi
(4) None of the above
.
.
Answer ▽ ✅Verified
(2) Central Drug Research Institute, Lucknow
BIRTH CONTROL
families by using various contraceptive methods.
An ideal contraceptive should be user-friendly, easily available,
effective and reversible with no or least side-effects. It also should in no
way interfere with the sexual drive, desire and/or the sexual act of the
user. A wide range of contraceptive methods are presently available which
could be broadly grouped into the following categories, namely
Natural/Traditional, Barrier, IUDs, Oral contraceptives, Injectables,
Implants and Surgical methods.
Natural methods work on the principle of avoiding chances of ovum
and sperms meeting. Periodic abstinence is one such method in which
the couples avoid or abstain from coitus from day 10 to 17 of the menstrual
cycle when ovulation could be expected. As chances of fertilisation are
very high during this period, it is called the fertile period. Therefore, by
abstaining from coitus during this period, conception could
be prevented. Withdrawal or coitus interruptus is another
method in which the male partner withdraws his penis from
the vagina just before ejaculation so as to avoid
insemination. Lactational amenorrhea (absence of
menstruation) method is based on the fact that ovulation
and therefore the cycle do not occur during the period of
intense lactation following parturition. Therefore, as long
as the mother breast-feeds the child fully, chances of
conception are almost nil. However, this method has been
reported to be effective only upto a maximum period of six
months following parturition. As no medicines or devices
are used in these methods, side effects are almost nil.
Chances of failure, though, of this method are also high.
In barrier methods, ovum and sperms are prevented
from physically meeting with the help of barriers. Such
methods are available for both males and females.
Condoms (Figure 4.1 a, b) are barriers made of thin rubber/
latex sheath that are used to cover the penis in the male or
vagina and cervix in the female, just before coitus so that
the ejaculated semen would not enter into the female
reproductive tract. This can prevent conception. ‘Nirodh’ is
a popular brand of condom for the male. Use of condoms
has increased in recent years due to its additional benefit of
protecting the user from contracting STIs and AIDS. Both
the male and the female condoms are disposable, can be
self-inserted and thereby gives privacy to the user.
Diaphragms, cervical caps and vaults are also barriers
made of rubber that are inserted into the female reproductive
tract to cover the cervix during coitus. They prevent
conception by blocking the entry of sperms through the
cervix. They are reusable. Spermicidal creams, jellies and
foams are usually used alongwith these barriers to increase
their contraceptive efficiency.
Another effective and popular method is the use of Intra Uterine
Devices (IUDs). These devices are inserted by doctors or expert nurses
in the uterus through vagina. These Intra Uterine Devices are presently
available as the non-medicated IUDs (e.g., Lippes loop), copper releasing
IUDs (CuT, Cu7, Multiload 375) and the hormone releasing IUDs
(Progestasert, LNG-20) (Figure 4.2). IUDs increase phagocytosis of sperms
within the uterus and the Cu ions released suppress sperm motility and
the fertilising capacity of sperms. The hormone releasing IUDs, in addition
make the uterus unsuitable for implantation and the
cervix hostile to the sperms. IUDs are ideal contraceptives
for the females who want to delay pregnancy and/or space
children. It is one of most widely accepted methods of
contraception in India.
Oral administration of small doses of either progestogens
or progestogen–estrogen combinations is another
contraceptive method used by the females. They are used
in the form of tablets and hence are popularly called the
pills. Pills have to be taken daily for a period of 21 days
starting preferably within the first five days of menstrual
cycle. After a gap of 7 days (during which menstruation
occurs) it has to be repeated in the same pattern till the female desires to
prevent conception. They inhibit ovulation and implantation as well as
alter the quality of cervical mucus to prevent/retard entry of sperms. Pills
are very effective with lesser side effects and are well accepted by the females.
Saheli –the new oral contraceptive for the females contains a non-steroidal
preparation. It is a ‘once a week’ pill with very few side effects and high
contraceptive value.by scientists at Central Drug Research Institute (CDRI) in Lucknow
Progestogens alone or in combination with estrogen can also be used
by females as injections or implants under the skin (Figure 4.3). Their
mode of action is similar to that of pills and their effective periods are
much longer. Administration of progestogens or progestogen-estrogen
combinations or IUDs within 72 hours of coitus have been found to be
very effective as emergency contraceptives as they could be used to avoid
possible pregnancy due to rape or casual unprotected intercourse.
Surgical methods, also called sterilisation, are generally advised for
the male/female partner as a terminal method
⬆️Prev____@organised notes_____Next⬇️
.What is the approximate world population according to the recent census? (May 2000):
(1) About 6 billion
(2) About 60 billion
(3) About 16 billion
(4) About 6 million
.
.
Answer ▽ ✅Verified
(1) About 6 billion
POPULATION STABILISATION AND BIRTH CONTROL
In the last century an all-round development in various fields significantly
improved the quality of life of the people. However, increased health
facilities along with better living conditions had an explosive impact on
the growth of population. The world population which was around
2 billion (2000 million) in 1900 rocketed to about 6 billion by 2000 and
7.2 billion in 2011. A similar trend was observed in India too. Our
population which was approximately 350 million at the time of our
independence reached close to the billion mark by 2000 and crossed
1.2 billion in May 2011. A rapid decline in death rate, maternal mortality
rate (MMR) and infant mortality rate (IMR) as well as an increase in
number of people in reproducible age are probable reasons for this.
Through our Reproductive Child Health (RCH) programme, though we
could bring down the population growth rate, it was only marginal.
According to the 2011 census report, the population growth rate was
less than 2 per cent, i.e., 20/1000/year, a rate at which our population
could increase rapidly. Such an alarming growth rate could lead to an
absolute scarcity of even the basic requirements, i.e., food, shelter and
clothing, in spite of significant progress made in those areas. Therefore,
the government was forced to take up serious measures to check this
population growth rate.
The most important step to overcome this problem is to motivate smaller
families by using various contraceptive methods. You might have seen
advertisements in the media as well as posters/bills, etc., showing a happy
couple with two children with a slogan Hum Do Hamare Do (we two, our
two). Many couples, mostly the young, urban, working ones have even
adopted an ‘one child norm’. Statutory raising of marriageable age of the
female to 18 years and that of males to 21 years, and incentives given to
couples with small families are two of the other measures taken to tackle
this problem. Let us describe some of the commonly used contraceptive
methods, which help prevent unwanted pregnancies.
⬆️Prev____@organised notes_____Next⬇️
.What is the approximate Indian population according to the recent census (May 2000)?
(1) About 1 billion
(2) About 1 million
(3) About 10 billion
(4) About 15 million
.
.
Answer ▽ ✅Verified
(1) About 1 billion
POPULATION STABILISATION AND BIRTH CONTROL
In the last century an all-round development in various fields significantly
improved the quality of life of the people. However, increased health
facilities along with better living conditions had an explosive impact on
the growth of population. The world population which was around
2 billion (2000 million) in 1900 rocketed to about 6 billion by 2000 and
7.2 billion in 2011. A similar trend was observed in India too. Our
population which was approximately 350 million at the time of our
independence reached close to the billion mark by 2000 and crossed
1.2 billion in May 2011. A rapid decline in death rate, maternal mortality
rate (MMR) and infant mortality rate (IMR) as well as an increase in
number of people in reproducible age are probable reasons for this.
Through our Reproductive Child Health (RCH) programme, though we
could bring down the population growth rate, it was only marginal.
According to the 2011 census report, the population growth rate was
less than 2 per cent, i.e., 20/1000/year, a rate at which our population
could increase rapidly. Such an alarming growth rate could lead to an
absolute scarcity of even the basic requirements, i.e., food, shelter and
clothing, in spite of significant progress made in those areas. Therefore,
the government was forced to take up serious measures to check this
population growth rate.
The most important step to overcome this problem is to motivate smaller
families by using various contraceptive methods. You might have seen
advertisements in the media as well as posters/bills, etc., showing a happy
couple with two children with a slogan Hum Do Hamare Do (we two, our
two). Many couples, mostly the young, urban, working ones have even
adopted an ‘one child norm’. Statutory raising of marriageable age of the
female to 18 years and that of males to 21 years, and incentives given to
couples with small families are two of the other measures taken to tackle
this problem. Let us describe some of the commonly used contraceptive
methods, which help prevent unwanted pregnancies.
⬆️Prev____@organised notes_____Next⬇️
.On which days of the menstrual cycle is ovulation expected?
1. 10th-30th
2. 1st-10th
3. 10th-17th
4. 18th-25th
.
.
Answer ▽ ✅Verified
3. 10th-17th
BIRTH CONTROL
families by using various contraceptive methods.
An ideal contraceptive should be user-friendly, easily available,
effective and reversible with no or least side-effects. It also should in no
way interfere with the sexual drive, desire and/or the sexual act of the
user. A wide range of contraceptive methods are presently available which
could be broadly grouped into the following categories, namely
Natural/Traditional, Barrier, IUDs, Oral contraceptives, Injectables,
Implants and Surgical methods.
Natural methods work on the principle of avoiding chances of ovum
and sperms meeting. Periodic abstinence is one such method in which
the couples avoid or abstain from coitus from day 10 to 17 of the menstrual
cycle when ovulation could be expected. As chances of fertilisation are
very high during this period, it is called the fertile period. Therefore, by
abstaining from coitus during this period, conception could
be prevented. Withdrawal or coitus interruptus is another
method in which the male partner withdraws his penis from
the vagina just before ejaculation so as to avoid
insemination. Lactational amenorrhea (absence of
menstruation) method is based on the fact that ovulation
and therefore the cycle do not occur during the period of
intense lactation following parturition. Therefore, as long
as the mother breast-feeds the child fully, chances of
conception are almost nil. However, this method has been
reported to be effective only upto a maximum period of six
months following parturition. As no medicines or devices
are used in these methods, side effects are almost nil.
Chances of failure, though, of this method are also high.
In barrier methods, ovum and sperms are prevented
from physically meeting with the help of barriers. Such
methods are available for both males and females.
Condoms (Figure 4.1 a, b) are barriers made of thin rubber/
latex sheath that are used to cover the penis in the male or
vagina and cervix in the female, just before coitus so that
the ejaculated semen would not enter into the female
reproductive tract. This can prevent conception. ‘Nirodh’ is
a popular brand of condom for the male. Use of condoms
has increased in recent years due to its additional benefit of
protecting the user from contracting STIs and AIDS. Both
the male and the female condoms are disposable, can be
self-inserted and thereby gives privacy to the user.
Diaphragms, cervical caps and vaults are also barriers
made of rubber that are inserted into the female reproductive
tract to cover the cervix during coitus. They prevent
conception by blocking the entry of sperms through the
cervix. They are reusable. Spermicidal creams, jellies and
foams are usually used alongwith these barriers to increase
their contraceptive efficiency.
Another effective and popular method is the use of Intra Uterine
Devices (IUDs). These devices are inserted by doctors or expert nurses
in the uterus through vagina. These Intra Uterine Devices are presently
available as the non-medicated IUDs (e.g., Lippes loop), copper releasing
IUDs (CuT, Cu7, Multiload 375) and the hormone releasing IUDs
(Progestasert, LNG-20) (Figure 4.2). IUDs increase phagocytosis of sperms
within the uterus and the Cu ions released suppress sperm motility and
the fertilising capacity of sperms. The hormone releasing IUDs, in addition
make the uterus unsuitable for implantation and the
cervix hostile to the sperms. IUDs are ideal contraceptives
for the females who want to delay pregnancy and/or space
children. It is one of most widely accepted methods of
contraception in India.
Oral administration of small doses of either progestogens
or progestogen–estrogen combinations is another
contraceptive method used by the females. They are used
in the form of tablets and hence are popularly called the
pills. Pills have to be taken daily for a period of 21 days
starting preferably within the first five days of menstrual
cycle. After a gap of 7 days (during which menstruation
occurs) it has to be repeated in the same pattern till the female desires to
prevent conception. They inhibit ovulation and implantation as well as
alter the quality of cervical mucus to prevent/retard entry of sperms. Pills
are very effective with lesser side effects and are well accepted by the females.
Saheli –the new oral contraceptive for the females contains a non-steroidal
preparation. It is a ‘once a week’ pill with very few side effects and high
contraceptive value.
Progestogens alone or in combination with estrogen can also be used
by females as injections or implants under the skin (Figure 4.3). Their
mode of action is similar to that of pills and their effective periods are
much longer. Administration of progestogens or progestogen-estrogen
combinations or IUDs within 72 hours of coitus have been found to be
very effective as emergency contraceptives as they could be used to avoid
possible pregnancy due to rape or casual unprotected intercourse.
Surgical methods, also called sterilisation, are generally advised for
the male/female partner as a terminal method
⬆️Prev____@organised notes_____Next⬇️
.Diaphragms, cervical caps and vaults are:
(1) Reusable
(2) Non-reusable
(3) Reusable for males only
(4) None of these
.
.
Answer ▽ ✅Verified
(1) Reusable
BIRTH CONTROL
families by using various contraceptive methods.
An ideal contraceptive should be user-friendly, easily available,
effective and reversible with no or least side-effects. It also should in no
way interfere with the sexual drive, desire and/or the sexual act of the
user. A wide range of contraceptive methods are presently available which
could be broadly grouped into the following categories, namely
Natural/Traditional, Barrier, IUDs, Oral contraceptives, Injectables,
Implants and Surgical methods.
Natural methods work on the principle of avoiding chances of ovum
and sperms meeting. Periodic abstinence is one such method in which
the couples avoid or abstain from coitus from day 10 to 17 of the menstrual
cycle when ovulation could be expected. As chances of fertilisation are
very high during this period, it is called the fertile period. Therefore, by
abstaining from coitus during this period, conception could
be prevented. Withdrawal or coitus interruptus is another
method in which the male partner withdraws his penis from
the vagina just before ejaculation so as to avoid
insemination. Lactational amenorrhea (absence of
menstruation) method is based on the fact that ovulation
and therefore the cycle do not occur during the period of
intense lactation following parturition. Therefore, as long
as the mother breast-feeds the child fully, chances of
conception are almost nil. However, this method has been
reported to be effective only upto a maximum period of six
months following parturition. As no medicines or devices
are used in these methods, side effects are almost nil.
Chances of failure, though, of this method are also high.
In barrier methods, ovum and sperms are prevented
from physically meeting with the help of barriers. Such
methods are available for both males and females.
Condoms (Figure 4.1 a, b) are barriers made of thin rubber/
latex sheath that are used to cover the penis in the male or
vagina and cervix in the female, just before coitus so that
the ejaculated semen would not enter into the female
reproductive tract. This can prevent conception. ‘Nirodh’ is
a popular brand of condom for the male. Use of condoms
has increased in recent years due to its additional benefit of
protecting the user from contracting STIs and AIDS. Both
the male and the female condoms are disposable, can be
self-inserted and thereby gives privacy to the user.
Diaphragms, cervical caps and vaults are also barriers
made of rubber that are inserted into the female reproductive
tract to cover the cervix during coitus. They prevent
conception by blocking the entry of sperms through the
cervix. They are reusable. Spermicidal creams, jellies and
foams are usually used alongwith these barriers to increase
their contraceptive efficiency.
Another effective and popular method is the use of Intra Uterine
Devices (IUDs). These devices are inserted by doctors or expert nurses
in the uterus through vagina. These Intra Uterine Devices are presently
available as the non-medicated IUDs (e.g., Lippes loop), copper releasing
IUDs (CuT, Cu7, Multiload 375) and the hormone releasing IUDs
(Progestasert, LNG-20) (Figure 4.2). IUDs increase phagocytosis of sperms
within the uterus and the Cu ions released suppress sperm motility and
the fertilising capacity of sperms. The hormone releasing IUDs, in addition
make the uterus unsuitable for implantation and the
cervix hostile to the sperms. IUDs are ideal contraceptives
for the females who want to delay pregnancy and/or space
children. It is one of most widely accepted methods of
contraception in India.
Oral administration of small doses of either progestogens
or progestogen–estrogen combinations is another
contraceptive method used by the females. They are used
in the form of tablets and hence are popularly called the
pills. Pills have to be taken daily for a period of 21 days
starting preferably within the first five days of menstrual
cycle. After a gap of 7 days (during which menstruation
occurs) it has to be repeated in the same pattern till the female desires to
prevent conception. They inhibit ovulation and implantation as well as
alter the quality of cervical mucus to prevent/retard entry of sperms. Pills
are very effective with lesser side effects and are well accepted by the females.
Saheli –the new oral contraceptive for the females contains a non-steroidal
preparation. It is a ‘once a week’ pill with very few side effects and high
contraceptive value.
Progestogens alone or in combination with estrogen can also be used
by females as injections or implants under the skin (Figure 4.3). Their
mode of action is similar to that of pills and their effective periods are
much longer. Administration of progestogens or progestogen-estrogen
combinations or IUDs within 72 hours of coitus have been found to be
very effective as emergency contraceptives as they could be used to avoid
possible pregnancy due to rape or casual unprotected intercourse.
Surgical methods, also called sterilisation, are generally advised for
the male/female partner as a terminal method
⬆️Prev____@organised notes_____Next⬇️
.What is true for IUDs?
I. They are self-inserted
II. They are inserted by expert nurses
III. They may be non-medicated IUDs, copper releasing IUDs or hormone releasing IUDs.
IV. They are the one of the most widely accepted contraceptives in India.
V. They are inter-uterine devices
(1) All of the above
(2) II; III, IV
(3) I, II, III
(4) I, II, III, V
.
.
Answer ▽ ✅Verified
(2) II; III, IV
(BIRTH CONTROL)
families by using various contraceptive methods.
An ideal contraceptive should be user-friendly, easily available,
effective and reversible with no or least side-effects. It also should in no
way interfere with the sexual drive, desire and/or the sexual act of the
user. A wide range of contraceptive methods are presently available which
could be broadly grouped into the following categories, namely
Natural/Traditional, Barrier, IUDs, Oral contraceptives, Injectables,
Implants and Surgical methods.
Natural methods work on the principle of avoiding chances of ovum
and sperms meeting. Periodic abstinence is one such method in which
the couples avoid or abstain from coitus from day 10 to 17 of the menstrual
cycle when ovulation could be expected. As chances of fertilisation are
very high during this period, it is called the fertile period. Therefore, by
abstaining from coitus during this period, conception could
be prevented. Withdrawal or coitus interruptus is another
method in which the male partner withdraws his penis from
the vagina just before ejaculation so as to avoid
insemination. Lactational amenorrhea (absence of
menstruation) method is based on the fact that ovulation
and therefore the cycle do not occur during the period of
intense lactation following parturition. Therefore, as long
as the mother breast-feeds the child fully, chances of
conception are almost nil. However, this method has been
reported to be effective only upto a maximum period of six
months following parturition. As no medicines or devices
are used in these methods, side effects are almost nil.
Chances of failure, though, of this method are also high.
In barrier methods, ovum and sperms are prevented
from physically meeting with the help of barriers. Such
methods are available for both males and females.
Condoms (Figure 4.1 a, b) are barriers made of thin rubber/
latex sheath that are used to cover the penis in the male or
vagina and cervix in the female, just before coitus so that
the ejaculated semen would not enter into the female
reproductive tract. This can prevent conception. ‘Nirodh’ is
a popular brand of condom for the male. Use of condoms
has increased in recent years due to its additional benefit of
protecting the user from contracting STIs and AIDS. Both
the male and the female condoms are disposable, can be
self-inserted and thereby gives privacy to the user.
Diaphragms, cervical caps and vaults are also barriers
made of rubber that are inserted into the female reproductive
tract to cover the cervix during coitus. They prevent
conception by blocking the entry of sperms through the
cervix. They are reusable. Spermicidal creams, jellies and
foams are usually used alongwith these barriers to increase
their contraceptive efficiency.
Another effective and popular method is the use of Intra Uterine
Devices (IUDs). These devices are inserted by doctors or expert nurses
in the uterus through vagina. These Intra Uterine Devices are presently
available as the non-medicated IUDs (e.g., Lippes loop), copper releasing
IUDs (CuT, Cu7, Multiload 375) and the hormone releasing IUDs
(Progestasert, LNG-20) (Figure 4.2). IUDs increase phagocytosis of sperms
within the uterus and the Cu ions released suppress sperm motility and
the fertilising capacity of sperms. The hormone releasing IUDs, in addition
make the uterus unsuitable for implantation and the
cervix hostile to the sperms. IUDs are ideal contraceptives
for the females who want to delay pregnancy and/or space
children. It is one of most widely accepted methods of
contraception in India.
Oral administration of small doses of either progestogens
or progestogen–estrogen combinations is another
contraceptive method used by the females. They are used
in the form of tablets and hence are popularly called the
pills. Pills have to be taken daily for a period of 21 days
starting preferably within the first five days of menstrual
cycle. After a gap of 7 days (during which menstruation
occurs) it has to be repeated in the same pattern till the female desires to
prevent conception. They inhibit ovulation and implantation as well as
alter the quality of cervical mucus to prevent/retard entry of sperms. Pills
are very effective with lesser side effects and are well accepted by the females.
Saheli –the new oral contraceptive for the females contains a non-steroidal
preparation. It is a ‘once a week’ pill with very few side effects and high
contraceptive value.
Progestogens alone or in combination with estrogen can also be used
by females as injections or implants under the skin (Figure 4.3). Their
mode of action is similar to that of pills and their effective periods are
much longer. Administration of progestogens or progestogen-estrogen
combinations or IUDs within 72 hours of coitus have been found to be
very effective as emergency contraceptives as they could be used to avoid
possible pregnancy due to rape or casual unprotected intercourse.
Surgical methods, also called sterilisation, are generally advised for
the male/female partner as a terminal method
⬆️Prev____@organised notes_____Next⬇️
.Pills:
I. Inhibit ovulation and implantation
II. Alter the quality of cervical mucus to prevent or retard the entry of sperms
III. Prevent the ejaculated semen from entering the female vagina
IV. Inhibit spermatogenesis
1. All of the above
2. I, II, III
3. I, II
4. I, III, IV
.
.
Answer ▽ ✅Verified
2. I, II, III
Pills have to be taken daily for a period of 21 days
starting preferably within the first five days of menstrual
cycle. After a gap of 7 days (during which menstruation
occurs) it has to be repeated in the same pattern till the female desires to
prevent conception. They inhibit ovulation and implantation as well as
alter the quality of cervical mucus to prevent/retard entry of sperms. Pills
are very effective with lesser side effects and are well accepted by the females.
Saheli –the new oral contraceptive for the females contains a non-steroidal
preparation. It is a ‘once a week’ pill with very few side effects and high
contraceptive value.
⬆️Prev____@organised notes_____Next⬇️
.What is true about "Saheli"?
I. Developed at the CDRI, Lucknow
II. Contains a steroidal preparation
III. Once-a-week" pill
IV. Many side effects
V. High contraceptive value
VI. Very few side effects
(1) I, II, III, V, VI
(2) I, III, V, VI
(3) I, II, III, IV, V
(4) I, III, IV, V
.
.
Answer ▽ ✅Verified
(2) I, III, V, VI
Pills have to be taken daily for a period of 21 days
starting preferably within the first five days of menstrual
cycle. After a gap of 7 days (during which menstruation
occurs) it has to be repeated in the same pattern till the female desires to
prevent conception. They inhibit ovulation and implantation as well as
alter the quality of cervical mucus to prevent/retard entry of sperms. Pills
are very effective with lesser side effects and are well accepted by the females.
Saheli –the new oral contraceptive for the females contains a non-steroidal
preparation. It is a ‘once a week’ pill with very few side effects and high
contraceptive value.
⬆️Prev____@organised notes_____Next⬇️
.MTP was legalised in India in:
(1) 1971
(2) 1951
(3) 1981
(4) 1923
.
.
Answer ▽ ✅Verified
(1) 1971
MEDICAL TERMINATION OF PREGNANCY (MTP)
medical termination of pregnancy (MTP) or induced abortion. Nearly
45 to 50 million MTPs are performed in a year all over the world which
accounts to 1/5th of the total number of conceived pregnancies in a year.
Whether to accept / legalise MTP or not is being debated upon in many
countries due to emotional, ethical, religious and social issues involved
in it. Government of India legalised MTP in 1971 with some strict conditions
to avoid its misuse. Such restrictions are all the more important to check
indiscriminate and illegal female foeticides which are reported to be high
in India.
Why MTP? Obviously the answer is–to get rid of unwanted
pregnancies either due to casual unprotected intercourse or failure of the
contraceptive used during coitus or rapes. MTPs are also essential in
certain cases where continuation of the pregnancy could be harmful or
even fatal either to the mother or to the foetus or both.
MTPs are considered relatively safe during the first trimester, i.e., upto
12 weeks of pregnancy. Second trimester abortions are much more riskier.
One disturbing trend observed is that a majority of the MTPs are performed
illegally by unqualified quacks which are not only unsafe but could be
fatal too. Another dangerous trend is the misuse of amniocentesis to
determine the sex of the unborn child. Frequently, if the foetus is found
to be female, it is followed by MTP- this is totally against what is legal.
The Medical Termination
of Pregnancy
(Amendment) Act, 2017
was enacted by the
government of India with
the intension of
reducing the incidence of
illegal abortion and
consequent maternal
mortality and morbidity.
According to this Act, a
pregnancy may be
terminated on certain
considered grounds
within the first 12 weeks
of pregnancy on the
opinion of one registered
medical practitioner. If
the pregnancy has lasted
more than 12 weeks, but
fewer than 24 weeks, two
registered medical
practitioners must be of
the opinion, formed in
good faith, that the
required ground exist.
The grounds for such
termination of
pregnancies are:
(i) The continuation of
the pregnancy would
involve a risk to the
life of the pregnant
woman or of grave
injury physical or
mental health; or
(ii There is a
substantial risk that
of the child were
born, it would suffer
from such physical
or mental
abnormalities as to
be seriously
handicapped.
Such practices should be avoided because these are dangerous both for
the young mother and the foetus. Effective counselling on the need to
avoid unprotected coitus and the risk factors involved in illegal abortions
as well as providing more health care facilities could reverse the mentioned
unhealthy trend.
⬆️Prev____@organised notes_____Next⬇️
.Which of the sets of diseases are completely curable if detected early?
(1) Hepatitis - B, Gonorrhoea, Syphilis
(2) Genital herpes, Chlamydiasis, Syphilis
(3) HIV Infections, Chlamydiasis, Gonorrhoea
(4) Chlamydiasis, Syphilis, Gonorrhoea
.
.
Answer ▽ ✅Verified
(4) Chlamydiasis, Syphilis, Gonorrhoea
Infections or diseases which are transmitted through sexual intercourse
are collectively called sexually transmitted infections (STI) or venereal
diseases (VD) or reproductive tract infections (RTI). Gonorrhoea, syphilis,
genital herpes, chlamydiasis, genital warts, trichomoniasis, hepatitis-B
and of course, the most discussed infection in the recent years, HIV leading
to AIDS are some of the common STIs. Among these, HIV infection is
most dangerous .
Some of these infections like hepatitis–B and HIV can also be
transmitted by sharing of injection needles, surgical instruments, etc.,
with infected persons, transfusion of blood, or from an infected mother to
the foetus too. Except for hepatitis-B, genital herpes and HIV infections,
other diseases are completely curable if detected early and treated
properly. Early symptoms of most of these are minor and include itching,
fluid discharge, slight pain, swellings, etc., in the genital region. Infected
females may often be asymptomatic and hence, may remain undetected
for long. Absence or less significant symptoms in the early stages of
infection and the social stigma attached to the STIs, deter the infected
persons from going for timely detection and proper treatment. This could
lead to complications later, which include pelvic inflammatory diseases
(PID), abortions, still births, ectopic pregnancies, infertility or even cancer
of the reproductive tract. STIs are a major threat to a healthy society.
Therefore, prevention or early detection and cure of these diseases are
given prime consideration under the reproductive health-care
programmes. Though all persons are vulnerable to these infections, their
incidences are reported to be very high among persons in the age group
of 15-24 years – the age group to which you also belong. There is no
reason to panic because prevention is possible. One could be free of these
infections by following the simple principles given below:
(i) Avoid sex with unknown partners/multiple partners.
(ii) Always try to use condoms during coitus.
(iii) In case of doubt, one should go to a qualified doctor for early
detection and get complete treatment if diagnosed with infection.
⬆️Prev____@organised notes_____Next⬇️
.Surgical methods of contraception prevent:
(1) Gamete formation
(2) Gamete motility
(3) Both (1) and (2)
(4) Spermatogenesis only
.
.
Answer ▽ ✅Verified
(2) Gamete motility
BIRTH CONTROL
families by using various contraceptive methods.
An ideal contraceptive should be user-friendly, easily available,
effective and reversible with no or least side-effects. It also should in no
way interfere with the sexual drive, desire and/or the sexual act of the
user. A wide range of contraceptive methods are presently available which
could be broadly grouped into the following categories, namely
Natural/Traditional, Barrier, IUDs, Oral contraceptives, Injectables,
Implants and Surgical methods.
Natural methods work on the principle of avoiding chances of ovum
and sperms meeting. Periodic abstinence is one such method in which
the couples avoid or abstain from coitus from day 10 to 17 of the menstrual
cycle when ovulation could be expected. As chances of fertilisation are
very high during this period, it is called the fertile period. Therefore, by
abstaining from coitus during this period, conception could
be prevented. Withdrawal or coitus interruptus is another
method in which the male partner withdraws his penis from
the vagina just before ejaculation so as to avoid
insemination. Lactational amenorrhea (absence of
menstruation) method is based on the fact that ovulation
and therefore the cycle do not occur during the period of
intense lactation following parturition. Therefore, as long
as the mother breast-feeds the child fully, chances of
conception are almost nil. However, this method has been
reported to be effective only upto a maximum period of six
months following parturition. As no medicines or devices
are used in these methods, side effects are almost nil.
Chances of failure, though, of this method are also high.
In barrier methods, ovum and sperms are prevented
from physically meeting with the help of barriers. Such
methods are available for both males and females.
Condoms (Figure 4.1 a, b) are barriers made of thin rubber/
latex sheath that are used to cover the penis in the male or
vagina and cervix in the female, just before coitus so that
the ejaculated semen would not enter into the female
reproductive tract. This can prevent conception. ‘Nirodh’ is
a popular brand of condom for the male. Use of condoms
has increased in recent years due to its additional benefit of
protecting the user from contracting STIs and AIDS. Both
the male and the female condoms are disposable, can be
self-inserted and thereby gives privacy to the user.
Diaphragms, cervical caps and vaults are also barriers
made of rubber that are inserted into the female reproductive
tract to cover the cervix during coitus. They prevent
conception by blocking the entry of sperms through the
cervix. They are reusable. Spermicidal creams, jellies and
foams are usually used alongwith these barriers to increase
their contraceptive efficiency.
Another effective and popular method is the use of Intra Uterine
Devices (IUDs). These devices are inserted by doctors or expert nurses
in the uterus through vagina. These Intra Uterine Devices are presently
available as the non-medicated IUDs (e.g., Lippes loop), copper releasing
IUDs (CuT, Cu7, Multiload 375) and the hormone releasing IUDs
(Progestasert, LNG-20) (Figure 4.2). IUDs increase phagocytosis of sperms
within the uterus and the Cu ions released suppress sperm motility and
the fertilising capacity of sperms. The hormone releasing IUDs, in addition
make the uterus unsuitable for implantation and the
cervix hostile to the sperms. IUDs are ideal contraceptives
for the females who want to delay pregnancy and/or space
children. It is one of most widely accepted methods of
contraception in India.
Oral administration of small doses of either progestogens
or progestogen–estrogen combinations is another
contraceptive method used by the females. They are used
in the form of tablets and hence are popularly called the
pills. Pills have to be taken daily for a period of 21 days
starting preferably within the first five days of menstrual
cycle. After a gap of 7 days (during which menstruation
occurs) it has to be repeated in the same pattern till the female desires to
prevent conception. They inhibit ovulation and implantation as well as
alter the quality of cervical mucus to prevent/retard entry of sperms. Pills
are very effective with lesser side effects and are well accepted by the females.
Saheli –the new oral contraceptive for the females contains a non-steroidal
preparation. It is a ‘once a week’ pill with very few side effects and high
contraceptive value.by scientists at Central Drug Research Institute (CDRI) in Lucknow
Progestogens alone or in combination with estrogen can also be used
by females as injections or implants under the skin (Figure 4.3). Their
mode of action is similar to that of pills and their effective periods are
much longer. Administration of progestogens or progestogen-estrogen
combinations or IUDs within 72 hours of coitus have been found to be
very effective as emergency contraceptives as they could be used to avoid
possible pregnancy due to rape or casual unprotected intercourse.
Surgical methods, also called sterilisation, are generally advised for
the male/female partner as a terminal method. Surgical intervention blocks
⬆️Prev____@organised notes_____Next⬇️
.What is false for GIFT?
(1) It is Gamete Intra-Fallopian Transfer
(2) Ovum from a donor is transferred into the oviduct of the recipient
(3) Zygote from a donor is transferred into the oviduct of the recipient
(4) The recipient cannot produce ovum
.
.
Answer ▽ ✅Verified
(3) Zygote from a donor is transferred into the oviduct of the recipient
INFERTILITY
infertility. A large number of couples all over the world including India
are infertile, i.e., they are unable to produce children inspite of unprotected
sexual co-habitation. The reasons for this could be many–physical,
congenital, diseases, drugs, immunological or even psychological.
In India, often the female is blamed for the couple being childless, but
more often than not, the problem lies in the male partner. Specialised
health care units (infertility clinics, etc.) could help in diagnosis and
corrective treatment of some of these disorders and enable these couples to
have children. However, where such corrections are not possible, the couples
could be assisted to have children through certain special techniques
commonly known as assisted reproductive technologies (ART).
In vitro fertilisation (IVF–fertilisation outside the body in almost
similar conditions as that in the body) followed by embryo transfer (ET)
is one of such methods. In this method, popularly known as test tube
baby programme, ova from the wife/donor (female) and sperms from the
husband/donor (male) are collected and are induced to form zygote under
simulated conditions in the laboratory. The zygote or early embryos (with
upto 8 blastomeres) could then be transferred into the fallopian tube
(ZIFT–zygote intra fallopian transfer) and embryos with more than
8 blastomeres, into the uterus (IUT – intra uterine transfer), to complete
its further development. Embryos formed by in-vivo fertilisation (fusion
of gametes within the female) also could be used for such transfer to assist
those females who cannot conceive.
Transfer of an ovum collected from a donor into the fallopian tube
(GIFT – gamete intra fallopian transfer) of another female who cannot
produce one, but can provide suitable environment for fertilisation and
further development is another method attempted. Intra cytoplasmic
sperm injection (ICSI) is another specialised procedure to form an embryo
in the laboratory in which a sperm is directly injected into the ovum.
Infertility cases either due to inability of the male partner to inseminate
the female or due to very low sperm counts in the ejaculates, could be
corrected by artificial insemination (AI) technique. In this technique,
the semen collected either from the husband or a healthy donor is artificially
introduced either into the vagina or into the uterus (IUI – intra-uterine
insemination) of the female.
Though options are many, all these techniques require extremely high
precision handling by specialised professionals and expensive
instrumentation. Therefore, these facilities are presently available only in
very few centres in the country. Obviously their benefits is affordable to
only a limited number of people. Emotional, religious and social factors
are also deterrents in the adoption of these methods. Since the ultimate
aim of all these procedures is to have children, in India we have so many
orphaned and destitute children, who would probably not survive till
maturity, unless taken care of. Our laws permit legal adoption and it is
as yet, one of the best methods for couples looking for parenthood.
⬆️Prev____@organised notes_____Next⬇️
.IUDs which are used by females:
(1) Are implanted under the skin and they release progestogen and estrogen
(2) Act as spermicidal jellies
(3) Release copper ions in the uterus that increase phagocytosis of sperm
(4) Block the entry of sperms into vagina.
.
.
Answer ▽ ✅Verified
(3) Release copper ions in the uterus that increase phagocytosis of sperm
⬆️Prev____@organised notes_____Next⬇️
.Which one of the following is the most widely accepted method of contraception in India, as at present?
1. IUDs' (Intra uterine devices)
2. Cervical caps
3. Tubectomy
4. Diaphragms
.
.
Answer ▽ ✅Verified
1. IUDs' (Intra uterine devices)
⬆️Prev____@organised notes_____Next⬇️
.Amenorrhea
1. will cause overdevelopment of the secondary sex characteristics
2. is never normal
3. is rare in women athletes due to their good physical conditioning
4. is the absence of menstruation
.
.
Answer ▽ ✅Verified
4. is the absence of menstruation
⬆️Prev____@organised notes_____Next⬇️
.Which of the following approaches does not give the defined action of contraceptive?
1. a
2. b
3. c
4. d
.
.
Answer ▽ ✅Verified
3. c
⬆️Prev____@organised notes_____Next⬇️
.Which of the following is a correct statement?
1. IUDs once inserted need not be replaced.
2. IUDs are generally inserted by the user herself.
3. IUDs increase phagocytosis of sperms in the uterus.
4. IUDs suppress gametogenesis.
.
.
Answer ▽ ✅Verified
3. IUDs increase phagocytosis of sperms in the uterus.
⬆️Prev____@organised notes_____Next⬇️
.Which of the following STDs are not curable?
1. Genital herpes, Hepatitis B, HIV infection
2. Chlamydiasis, Syphilis, Genital warts
3. HIV, Gonorrhoea, Trichomoniasis
4. Gonorrhoea, Trichomoniasis, Hepatitis B
.
.
Answer ▽ ✅Verified
1. Genital herpes, Hepatitis B, HIV infection
⬆️Prev____@organised notes_____Next⬇️
.The test-tube baby programme employs which one of the following techniques?
1. Intra Cytoplasmic Sperm Injection (ICSI)
2. Intra Uterine Insemination (IUI)
3. Gamete Intra Fallopian Transfer (GIFT)
4. Zygote Intra Fallopian Transfer (ZIFT)
.
.
Answer ▽ ✅Verified
4. Zygote Intra Fallopian Transfer (ZIFT)
INFERTILITY
infertility. A large number of couples all over the world including India
are infertile, i.e., they are unable to produce children inspite of unprotected
sexual co-habitation. The reasons for this could be many–physical,
congenital, diseases, drugs, immunological or even psychological.
In India, often the female is blamed for the couple being childless, but
more often than not, the problem lies in the male partner. Specialised
health care units (infertility clinics, etc.) could help in diagnosis and
corrective treatment of some of these disorders and enable these couples to
have children. However, where such corrections are not possible, the couples
could be assisted to have children through certain special techniques
commonly known as assisted reproductive technologies (ART).
In vitro fertilisation (IVF–fertilisation outside the body in almost
similar conditions as that in the body) followed by embryo transfer (ET)
is one of such methods. In this method, popularly known as test tube
baby programme, ova from the wife/donor (female) and sperms from the
husband/donor (male) are collected and are induced to form zygote under
simulated conditions in the laboratory. The zygote or early embryos (with
upto 8 blastomeres) could then be transferred into the fallopian tube
(ZIFT–zygote intra fallopian transfer) and embryos with more than
8 blastomeres, into the uterus (IUT – intra uterine transfer), to complete
its further development. Embryos formed by in-vivo fertilisation (fusion
of gametes within the female) also could be used for such transfer to assist
those females who cannot conceive.
Transfer of an ovum collected from a donor into the fallopian tube
(GIFT – gamete intra fallopian transfer) of another female who cannot
produce one, but can provide suitable environment for fertilisation and
further development is another method attempted. Intra cytoplasmic
sperm injection (ICSI) is another specialised procedure to form an embryo
in the laboratory in which a sperm is directly injected into the ovum.
Infertility cases either due to inability of the male partner to inseminate
the female or due to very low sperm counts in the ejaculates, could be
corrected by artificial insemination (AI) technique. In this technique,
the semen collected either from the husband or a healthy donor is artificially
introduced either into the vagina or into the uterus (IUI – intra-uterine
insemination) of the female.
Though options are many, all these techniques require extremely high
precision handling by specialised professionals and expensive
instrumentation. Therefore, these facilities are presently available only in
very few centres in the country. Obviously their benefits is affordable to
only a limited number of people. Emotional, religious and social factors
are also deterrents in the adoption of these methods. Since the ultimate
aim of all these procedures is to have children, in India we have so many
orphaned and destitute children, who would probably not survive till
maturity, unless taken care of. Our laws permit legal adoption and it is
as yet, one of the best methods for couples looking for parenthood.
⬆️Prev____@organised notes_____Next⬇️
.Contraceptive oral pills help in birth control by
(1) killing the sperms in uterus
(2) preventing implantation
(3) preventing ovulation
(4) both (b) and (c).
.
.
Answer ▽ ✅Verified
(4) both (b) and (c).
BIRTH CONTROL
families by using various contraceptive methods.
An ideal contraceptive should be user-friendly, easily available,
effective and reversible with no or least side-effects. It also should in no
way interfere with the sexual drive, desire and/or the sexual act of the
user. A wide range of contraceptive methods are presently available which
could be broadly grouped into the following categories, namely
Natural/Traditional, Barrier, IUDs, Oral contraceptives, Injectables,
Implants and Surgical methods.
Natural methods work on the principle of avoiding chances of ovum
and sperms meeting. Periodic abstinence is one such method in which
the couples avoid or abstain from coitus from day 10 to 17 of the menstrual
cycle when ovulation could be expected. As chances of fertilisation are
very high during this period, it is called the fertile period. Therefore, by
abstaining from coitus during this period, conception could
be prevented. Withdrawal or coitus interruptus is another
method in which the male partner withdraws his penis from
the vagina just before ejaculation so as to avoid
insemination. Lactational amenorrhea (absence of
menstruation) method is based on the fact that ovulation
and therefore the cycle do not occur during the period of
intense lactation following parturition. Therefore, as long
as the mother breast-feeds the child fully, chances of
conception are almost nil. However, this method has been
reported to be effective only upto a maximum period of six
months following parturition. As no medicines or devices
are used in these methods, side effects are almost nil.
Chances of failure, though, of this method are also high.
In barrier methods, ovum and sperms are prevented
from physically meeting with the help of barriers. Such
methods are available for both males and females.
Condoms (Figure 4.1 a, b) are barriers made of thin rubber/
latex sheath that are used to cover the penis in the male or
vagina and cervix in the female, just before coitus so that
the ejaculated semen would not enter into the female
reproductive tract. This can prevent conception. ‘Nirodh’ is
a popular brand of condom for the male. Use of condoms
has increased in recent years due to its additional benefit of
protecting the user from contracting STIs and AIDS. Both
the male and the female condoms are disposable, can be
self-inserted and thereby gives privacy to the user.
Diaphragms, cervical caps and vaults are also barriers
made of rubber that are inserted into the female reproductive
tract to cover the cervix during coitus. They prevent
conception by blocking the entry of sperms through the
cervix. They are reusable. Spermicidal creams, jellies and
foams are usually used alongwith these barriers to increase
their contraceptive efficiency.
Another effective and popular method is the use of Intra Uterine
Devices (IUDs). These devices are inserted by doctors or expert nurses
in the uterus through vagina. These Intra Uterine Devices are presently
available as the non-medicated IUDs (e.g., Lippes loop), copper releasing
IUDs (CuT, Cu7, Multiload 375) and the hormone releasing IUDs
(Progestasert, LNG-20) (Figure 4.2). IUDs increase phagocytosis of sperms
within the uterus and the Cu ions released suppress sperm motility and
the fertilising capacity of sperms. The hormone releasing IUDs, in addition
make the uterus unsuitable for implantation and the
cervix hostile to the sperms. IUDs are ideal contraceptives
for the females who want to delay pregnancy and/or space
children. It is one of most widely accepted methods of
contraception in India.
Oral administration of small doses of either progestogens
or progestogen–estrogen combinations is another
contraceptive method used by the females. They are used
in the form of tablets and hence are popularly called the
pills. Pills have to be taken daily for a period of 21 days
starting preferably within the first five days of menstrual
cycle. After a gap of 7 days (during which menstruation
occurs) it has to be repeated in the same pattern till the female desires to
prevent conception. They inhibit ovulation and implantation as well as
alter the quality of cervical mucus to prevent/retard entry of sperms. Pills
are very effective with lesser side effects and are well accepted by the females.
Saheli –the new oral contraceptive for the females contains a non-steroidal
preparation. It is a ‘once a week’ pill with very few side effects and high
contraceptive value.
Progestogens alone or in combination with estrogen can also be used
by females as injections or implants under the skin (Figure 4.3). Their
mode of action is similar to that of pills and their effective periods are
much longer. Administration of progestogens or progestogen-estrogen
combinations or IUDs within 72 hours of coitus have been found to be
very effective as emergency contraceptives as they could be used to avoid
possible pregnancy due to rape or casual unprotected intercourse.
Surgical methods, also called sterilisation, are generally advised for
the male/female partner as a terminal method
⬆️Prev____@organised notes_____Next⬇️
.When were family planning programmes initiated in India?
(1) 1948
(2) 1962
(3) 1959
(4) 1951
.
.
Answer ▽ ✅Verified
(4) 1951
India was amongst the first countries in the world to
initiate action plans and programmes at a national level
to attain total reproductive health as a social goal.
These programmes called ‘family planning’ were
initiated in 1951 and were periodically assessed over
the past decades. Improved programmes covering wider
reproduction-related areas are currently in operation under the
popular name ‘Reproductive and Child Health Care (RCH) programmes’.
Creating awareness among people about various reproduction related
aspects and providing facilities and support for building up a
reproductively healthy society are the major tasks under these
programmes.
With the help of audio-visual and the print-media governmental and
non-governmental agencies have taken various steps to create awareness
among the people about reproduction-related aspects. Parents, other
close relatives, teachers and friends, also have a major role in the
dissemination of the above information. Introduction of sex education
in schools should also be encouraged to provide right information to
the young so as to discourage children from believing in myths and
having misconceptions about sex-related aspects. Proper information
about reproductive organs, adolescence and related changes, safe and
hygienic sexual practices, sexually transmitted diseases (STD), AIDS,
etc., would help people, especially those in the adolescent age group to
lead a reproductively healthy life. Educating people, especially fertile
couples and those in marriageable age group, about available birth
control options, care of pregnant mothers, post-natal care of the mother
and child, importance of breast feeding, equal opportunities for the male
and the female child, etc., would address the importance of bringing up
socially conscious healthy families of desired size. Awareness of problems
due to uncontrolled population growth, social evils like sex-abuse and
sex-related crimes, etc., need to be created to enable people to think
and take up necessary steps to prevent them and thereby build up a
socially responsible and healthy society.
⬆️Prev____@organised notes_____Next⬇️
.What is the full form of RCH?
(1) Reproductive and Child Health Care
(2) Reproduction, Contraception and Health
(3) Reproduction and Child Health
(4) None of these
.
.
Answer ▽ ✅Verified
(1) Reproductive and Child Health Care
India was amongst the first countries in the world to
initiate action plans and programmes at a national level
to attain total reproductive health as a social goal.
These programmes called ‘family planning’ were
initiated in 1951 and were periodically assessed over
the past decades. Improved programmes covering wider
reproduction-related areas are currently in operation under the
popular name ‘Reproductive and Child Health Care (RCH) programmes’.
Creating awareness among people about various reproduction related
aspects and providing facilities and support for building up a
reproductively healthy society are the major tasks under these
programmes.
With the help of audio-visual and the print-media governmental and
non-governmental agencies have taken various steps to create awareness
among the people about reproduction-related aspects. Parents, other
close relatives, teachers and friends, also have a major role in the
dissemination of the above information. Introduction of sex education
in schools should also be encouraged to provide right information to
the young so as to discourage children from believing in myths and
having misconceptions about sex-related aspects. Proper information
about reproductive organs, adolescence and related changes, safe and
hygienic sexual practices, sexually transmitted diseases (STD), AIDS,
etc., would help people, especially those in the adolescent age group to
lead a reproductively healthy life. Educating people, especially fertile
couples and those in marriageable age group, about available birth
control options, care of pregnant mothers, post-natal care of the mother
and child, importance of breast feeding, equal opportunities for the male
and the female child, etc., would address the importance of bringing up
socially conscious healthy families of desired size. Awareness of problems
due to uncontrolled population growth, social evils like sex-abuse and
sex-related crimes, etc., need to be created to enable people to think
and take up necessary steps to prevent them and thereby build up a
socially responsible and healthy society.
⬆️Prev____@organised notes_____Next⬇️
.Where was "Saheli" developed?
(1) Indian Council of Medical Research, New Delhi
(2) Central Drug Research Institute, Lucknow
(3) All India Institute of Medical Sciences, New Delhi
(4) None of the above
.
.
Answer ▽ ✅Verified
(2) Central Drug Research Institute, Lucknow
BIRTH CONTROL
families by using various contraceptive methods.
An ideal contraceptive should be user-friendly, easily available,
effective and reversible with no or least side-effects. It also should in no
way interfere with the sexual drive, desire and/or the sexual act of the
user. A wide range of contraceptive methods are presently available which
could be broadly grouped into the following categories, namely
Natural/Traditional, Barrier, IUDs, Oral contraceptives, Injectables,
Implants and Surgical methods.
Natural methods work on the principle of avoiding chances of ovum
and sperms meeting. Periodic abstinence is one such method in which
the couples avoid or abstain from coitus from day 10 to 17 of the menstrual
cycle when ovulation could be expected. As chances of fertilisation are
very high during this period, it is called the fertile period. Therefore, by
abstaining from coitus during this period, conception could
be prevented. Withdrawal or coitus interruptus is another
method in which the male partner withdraws his penis from
the vagina just before ejaculation so as to avoid
insemination. Lactational amenorrhea (absence of
menstruation) method is based on the fact that ovulation
and therefore the cycle do not occur during the period of
intense lactation following parturition. Therefore, as long
as the mother breast-feeds the child fully, chances of
conception are almost nil. However, this method has been
reported to be effective only upto a maximum period of six
months following parturition. As no medicines or devices
are used in these methods, side effects are almost nil.
Chances of failure, though, of this method are also high.
In barrier methods, ovum and sperms are prevented
from physically meeting with the help of barriers. Such
methods are available for both males and females.
Condoms (Figure 4.1 a, b) are barriers made of thin rubber/
latex sheath that are used to cover the penis in the male or
vagina and cervix in the female, just before coitus so that
the ejaculated semen would not enter into the female
reproductive tract. This can prevent conception. ‘Nirodh’ is
a popular brand of condom for the male. Use of condoms
has increased in recent years due to its additional benefit of
protecting the user from contracting STIs and AIDS. Both
the male and the female condoms are disposable, can be
self-inserted and thereby gives privacy to the user.
Diaphragms, cervical caps and vaults are also barriers
made of rubber that are inserted into the female reproductive
tract to cover the cervix during coitus. They prevent
conception by blocking the entry of sperms through the
cervix. They are reusable. Spermicidal creams, jellies and
foams are usually used alongwith these barriers to increase
their contraceptive efficiency.
Another effective and popular method is the use of Intra Uterine
Devices (IUDs). These devices are inserted by doctors or expert nurses
in the uterus through vagina. These Intra Uterine Devices are presently
available as the non-medicated IUDs (e.g., Lippes loop), copper releasing
IUDs (CuT, Cu7, Multiload 375) and the hormone releasing IUDs
(Progestasert, LNG-20) (Figure 4.2). IUDs increase phagocytosis of sperms
within the uterus and the Cu ions released suppress sperm motility and
the fertilising capacity of sperms. The hormone releasing IUDs, in addition
make the uterus unsuitable for implantation and the
cervix hostile to the sperms. IUDs are ideal contraceptives
for the females who want to delay pregnancy and/or space
children. It is one of most widely accepted methods of
contraception in India.
Oral administration of small doses of either progestogens
or progestogen–estrogen combinations is another
contraceptive method used by the females. They are used
in the form of tablets and hence are popularly called the
pills. Pills have to be taken daily for a period of 21 days
starting preferably within the first five days of menstrual
cycle. After a gap of 7 days (during which menstruation
occurs) it has to be repeated in the same pattern till the female desires to
prevent conception. They inhibit ovulation and implantation as well as
alter the quality of cervical mucus to prevent/retard entry of sperms. Pills
are very effective with lesser side effects and are well accepted by the females.
Saheli –the new oral contraceptive for the females contains a non-steroidal
preparation. It is a ‘once a week’ pill with very few side effects and high
contraceptive value.by scientists at Central Drug Research Institute (CDRI) in Lucknow
Progestogens alone or in combination with estrogen can also be used
by females as injections or implants under the skin (Figure 4.3). Their
mode of action is similar to that of pills and their effective periods are
much longer. Administration of progestogens or progestogen-estrogen
combinations or IUDs within 72 hours of coitus have been found to be
very effective as emergency contraceptives as they could be used to avoid
possible pregnancy due to rape or casual unprotected intercourse.
Surgical methods, also called sterilisation, are generally advised for
the male/female partner as a terminal method
⬆️Prev____@organised notes_____Next⬇️
.What is the approximate world population according to the recent census? (May 2000):
(1) About 6 billion
(2) About 60 billion
(3) About 16 billion
(4) About 6 million
.
.
Answer ▽ ✅Verified
(1) About 6 billion
POPULATION STABILISATION AND BIRTH CONTROL
In the last century an all-round development in various fields significantly
improved the quality of life of the people. However, increased health
facilities along with better living conditions had an explosive impact on
the growth of population. The world population which was around
2 billion (2000 million) in 1900 rocketed to about 6 billion by 2000 and
7.2 billion in 2011. A similar trend was observed in India too. Our
population which was approximately 350 million at the time of our
independence reached close to the billion mark by 2000 and crossed
1.2 billion in May 2011. A rapid decline in death rate, maternal mortality
rate (MMR) and infant mortality rate (IMR) as well as an increase in
number of people in reproducible age are probable reasons for this.
Through our Reproductive Child Health (RCH) programme, though we
could bring down the population growth rate, it was only marginal.
According to the 2011 census report, the population growth rate was
less than 2 per cent, i.e., 20/1000/year, a rate at which our population
could increase rapidly. Such an alarming growth rate could lead to an
absolute scarcity of even the basic requirements, i.e., food, shelter and
clothing, in spite of significant progress made in those areas. Therefore,
the government was forced to take up serious measures to check this
population growth rate.
The most important step to overcome this problem is to motivate smaller
families by using various contraceptive methods. You might have seen
advertisements in the media as well as posters/bills, etc., showing a happy
couple with two children with a slogan Hum Do Hamare Do (we two, our
two). Many couples, mostly the young, urban, working ones have even
adopted an ‘one child norm’. Statutory raising of marriageable age of the
female to 18 years and that of males to 21 years, and incentives given to
couples with small families are two of the other measures taken to tackle
this problem. Let us describe some of the commonly used contraceptive
methods, which help prevent unwanted pregnancies.
⬆️Prev____@organised notes_____Next⬇️
.What is the approximate Indian population according to the recent census (May 2000)?
(1) About 1 billion
(2) About 1 million
(3) About 10 billion
(4) About 15 million
.
.
Answer ▽ ✅Verified
(1) About 1 billion
POPULATION STABILISATION AND BIRTH CONTROL
In the last century an all-round development in various fields significantly
improved the quality of life of the people. However, increased health
facilities along with better living conditions had an explosive impact on
the growth of population. The world population which was around
2 billion (2000 million) in 1900 rocketed to about 6 billion by 2000 and
7.2 billion in 2011. A similar trend was observed in India too. Our
population which was approximately 350 million at the time of our
independence reached close to the billion mark by 2000 and crossed
1.2 billion in May 2011. A rapid decline in death rate, maternal mortality
rate (MMR) and infant mortality rate (IMR) as well as an increase in
number of people in reproducible age are probable reasons for this.
Through our Reproductive Child Health (RCH) programme, though we
could bring down the population growth rate, it was only marginal.
According to the 2011 census report, the population growth rate was
less than 2 per cent, i.e., 20/1000/year, a rate at which our population
could increase rapidly. Such an alarming growth rate could lead to an
absolute scarcity of even the basic requirements, i.e., food, shelter and
clothing, in spite of significant progress made in those areas. Therefore,
the government was forced to take up serious measures to check this
population growth rate.
The most important step to overcome this problem is to motivate smaller
families by using various contraceptive methods. You might have seen
advertisements in the media as well as posters/bills, etc., showing a happy
couple with two children with a slogan Hum Do Hamare Do (we two, our
two). Many couples, mostly the young, urban, working ones have even
adopted an ‘one child norm’. Statutory raising of marriageable age of the
female to 18 years and that of males to 21 years, and incentives given to
couples with small families are two of the other measures taken to tackle
this problem. Let us describe some of the commonly used contraceptive
methods, which help prevent unwanted pregnancies.
⬆️Prev____@organised notes_____Next⬇️
.On which days of the menstrual cycle is ovulation expected?
1. 10th-30th
2. 1st-10th
3. 10th-17th
4. 18th-25th
.
.
Answer ▽ ✅Verified
3. 10th-17th
BIRTH CONTROL
families by using various contraceptive methods.
An ideal contraceptive should be user-friendly, easily available,
effective and reversible with no or least side-effects. It also should in no
way interfere with the sexual drive, desire and/or the sexual act of the
user. A wide range of contraceptive methods are presently available which
could be broadly grouped into the following categories, namely
Natural/Traditional, Barrier, IUDs, Oral contraceptives, Injectables,
Implants and Surgical methods.
Natural methods work on the principle of avoiding chances of ovum
and sperms meeting. Periodic abstinence is one such method in which
the couples avoid or abstain from coitus from day 10 to 17 of the menstrual
cycle when ovulation could be expected. As chances of fertilisation are
very high during this period, it is called the fertile period. Therefore, by
abstaining from coitus during this period, conception could
be prevented. Withdrawal or coitus interruptus is another
method in which the male partner withdraws his penis from
the vagina just before ejaculation so as to avoid
insemination. Lactational amenorrhea (absence of
menstruation) method is based on the fact that ovulation
and therefore the cycle do not occur during the period of
intense lactation following parturition. Therefore, as long
as the mother breast-feeds the child fully, chances of
conception are almost nil. However, this method has been
reported to be effective only upto a maximum period of six
months following parturition. As no medicines or devices
are used in these methods, side effects are almost nil.
Chances of failure, though, of this method are also high.
In barrier methods, ovum and sperms are prevented
from physically meeting with the help of barriers. Such
methods are available for both males and females.
Condoms (Figure 4.1 a, b) are barriers made of thin rubber/
latex sheath that are used to cover the penis in the male or
vagina and cervix in the female, just before coitus so that
the ejaculated semen would not enter into the female
reproductive tract. This can prevent conception. ‘Nirodh’ is
a popular brand of condom for the male. Use of condoms
has increased in recent years due to its additional benefit of
protecting the user from contracting STIs and AIDS. Both
the male and the female condoms are disposable, can be
self-inserted and thereby gives privacy to the user.
Diaphragms, cervical caps and vaults are also barriers
made of rubber that are inserted into the female reproductive
tract to cover the cervix during coitus. They prevent
conception by blocking the entry of sperms through the
cervix. They are reusable. Spermicidal creams, jellies and
foams are usually used alongwith these barriers to increase
their contraceptive efficiency.
Another effective and popular method is the use of Intra Uterine
Devices (IUDs). These devices are inserted by doctors or expert nurses
in the uterus through vagina. These Intra Uterine Devices are presently
available as the non-medicated IUDs (e.g., Lippes loop), copper releasing
IUDs (CuT, Cu7, Multiload 375) and the hormone releasing IUDs
(Progestasert, LNG-20) (Figure 4.2). IUDs increase phagocytosis of sperms
within the uterus and the Cu ions released suppress sperm motility and
the fertilising capacity of sperms. The hormone releasing IUDs, in addition
make the uterus unsuitable for implantation and the
cervix hostile to the sperms. IUDs are ideal contraceptives
for the females who want to delay pregnancy and/or space
children. It is one of most widely accepted methods of
contraception in India.
Oral administration of small doses of either progestogens
or progestogen–estrogen combinations is another
contraceptive method used by the females. They are used
in the form of tablets and hence are popularly called the
pills. Pills have to be taken daily for a period of 21 days
starting preferably within the first five days of menstrual
cycle. After a gap of 7 days (during which menstruation
occurs) it has to be repeated in the same pattern till the female desires to
prevent conception. They inhibit ovulation and implantation as well as
alter the quality of cervical mucus to prevent/retard entry of sperms. Pills
are very effective with lesser side effects and are well accepted by the females.
Saheli –the new oral contraceptive for the females contains a non-steroidal
preparation. It is a ‘once a week’ pill with very few side effects and high
contraceptive value.
Progestogens alone or in combination with estrogen can also be used
by females as injections or implants under the skin (Figure 4.3). Their
mode of action is similar to that of pills and their effective periods are
much longer. Administration of progestogens or progestogen-estrogen
combinations or IUDs within 72 hours of coitus have been found to be
very effective as emergency contraceptives as they could be used to avoid
possible pregnancy due to rape or casual unprotected intercourse.
Surgical methods, also called sterilisation, are generally advised for
the male/female partner as a terminal method
⬆️Prev____@organised notes____End⬇️